On the occasion of International Hereditary Angioedema (HAE) Awareness Day, the Romanian Society of Allergology and Clinical Immunology (RSACI) draws attention to a rare, underdiagnosed condition often mistaken for common allergies: hereditary angioedema – a genetic disease that can become fatal without treatment.
What is hereditary angioedema?
Hereditary angioedema (HAE) is a very rare and potentially life-threatening genetic condition, occurring in approximately 1 in 10,000 to 1 in 50,000 people. HAE is characterized by recurrent episodes of swelling (edema) affecting the skin, mucous membranes, airways, and internal organs. HAE attacks can last several days and, in the case of laryngeal edema, can be fatal if not treated promptly.
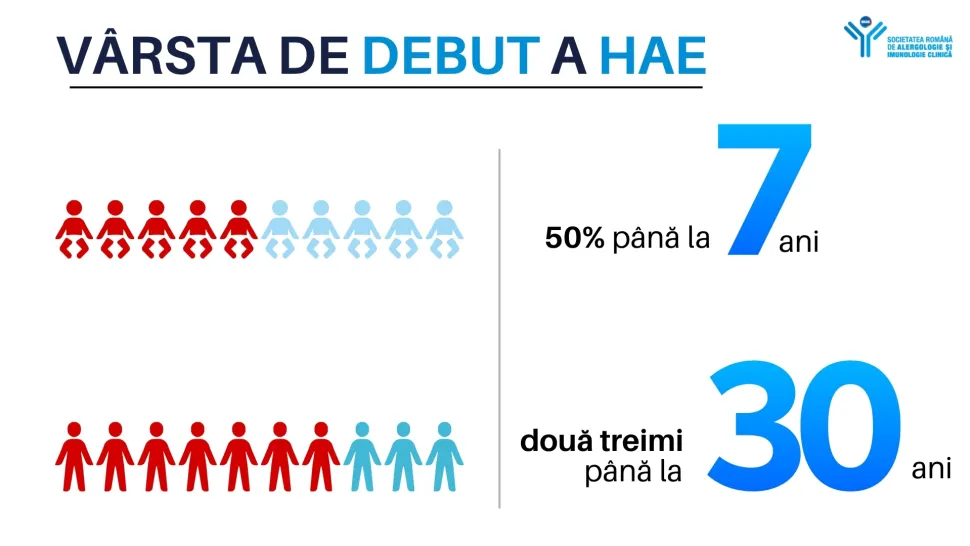
The age of onset of hereditary angioedema (HAE) varies considerably. Studies show that half of patients report symptoms by the age of seven, and over two-thirds become symptomatic by the age of thirteen. An increased frequency of attacks is also observed during puberty or adolescence.
Causes and Transmission
HAE is caused by a genetic mutation that affects the production or functionality of C1 inhibitor, a protein involved in regulating inflammation. This can lead to a biochemical imbalance that produces unwanted peptides, causing capillaries to release fluid into surrounding tissues and resulting in edema.
HAE is inherited in an autosomal dominant manner, meaning an affected parent has a 50% chance of passing the condition to their child. However, approximately 25% of cases arise from spontaneous mutations, without any family history.
The challenges of the diagnostic
Although hereditary angioedema (HAE) is a rare form of angioedema, most episodes of swelling are not caused by this disease. In the majority of cases, edema results from allergic reactions or other mechanisms that do not involve a C1 inhibitor deficiency.
Unlike allergic angioedema, HAE does not respond to antihistamines or corticosteroids, which is why an accurate diagnosis relies on specific laboratory tests (measuring C1 inhibitor and serum C4) and/or genetic testing. The most common forms are:
HAE Type I – 85% of cases, with low C1 inhibitor levels.
HAE Type II – 15% of cases, with normal but non-functional C1 inhibitor.
HAE with normal C1 inhibitor – a recently identified form, still considered hereditary. In women, episodes can be triggered or worsened by pregnancy or the use of oral contraceptives. However, affected men have also been identified in the same families, supporting the genetic nature of the disease
Modern treatment exists – but access is essential!
Although hereditary angioedema has no cure, modern treatments can effectively control the disease, prevent attacks, and reduce the risk of serious complications. It is crucial for patients to have access to both emergency and prophylactic therapies, as well as a personalized management plan."
"Because hereditary angioedema is so rare, it is often misdiagnosed, and standard treatments do not work. That’s why it is vital for physicians to recognize the disease quickly and collaborate with patients and authorities for accurate diagnosis and modern treatments that can change lives. Fortunately, there is also good news. Treatments for hereditary angioedema have advanced tremendously: there are now solutions that stop attacks and can prevent them, and gene therapies in development promise, one day, to correct the very cause of the disease," says Prof. Dr. Asli Akkor, President of NAIS (National Allergy Immunology Society).
On-demand’ treatment (or emergency treatment) aims to stop the progression of edema and rapidly relieve symptoms. Prompt administration of this type of treatment is especially crucial for edema affecting the throat or airways. If such an attack is not treated in time, it can lead to suffocation and death.
The specific medications available and recommended for “on-demand” treatment (or acute attack treatment) in hereditary angioedema (HAE) include:
- Intravenous C1 inhibitor concentrate
- Plasma-derived products (pdC1-inhibitor concentrate)
- Genetically engineered products (recombinant or rhC1-inhibitor concentrate, not derived from plasma)
- Bradykinin receptor antagonist
- Icatibant"
“Long-term prophylaxis (LTP) refers to the regular use of medication to prevent angioedema attacks in patients with hereditary angioedema (HAE). The goal of this therapy is to reduce the frequency of attacks, and some modern medications can even completely prevent them," says Assistant Professor Dr. Valentin Iovin, Secretary General of SRAIC.
It is important to note that even patients on prophylactic treatment may still experience attacks, which is why all individuals with HAE must also have immediate access to ‘on-demand’ (emergency) treatment.
In recent years, several modern therapies have been approved for long-term prophylaxis of HAE. Recommended options include:**
- C1 inhibitor concentrate, including plasma-derived variants (pdC1-inhibitor)
- Plasma kallikrein inhibitors, such as:
- Lanadelumab
- Berotralstat (recently available in Romania)
These treatments provide a real chance for HAE patients to live with fewer limitations and significantly reduce the risks associated with the disease.
“Without proper treatment, a hereditary angioedema attack can be fatal. It is essential that this rare disease is recognized, correctly diagnosed, and appropriately treated. Early diagnosis and adequate treatment can save lives. It is our responsibility, as specialists in allergology and clinical immunology, to raise awareness of this disease and improve patients’ quality of life,” says Assistant Professor Dr. Valentin Iovin, Secretary General of SRAIC.
Call to authorities and physicians
RSACI supports equitable access to diagnosis, treatment, and continuing medical education, and encourages collaboration among physicians, patients, and authorities for an integrated approach to rare diseases.
Awareness campaign carried out with the support of Takeda

Stay up to date with the latest news: key events, industry insights, trends in medical communication, and strategic insights. Subscribe and stay connected to the pulse of the medical field.
